Stem Cell Therapy for ACL Injuries: What Patients Should Know
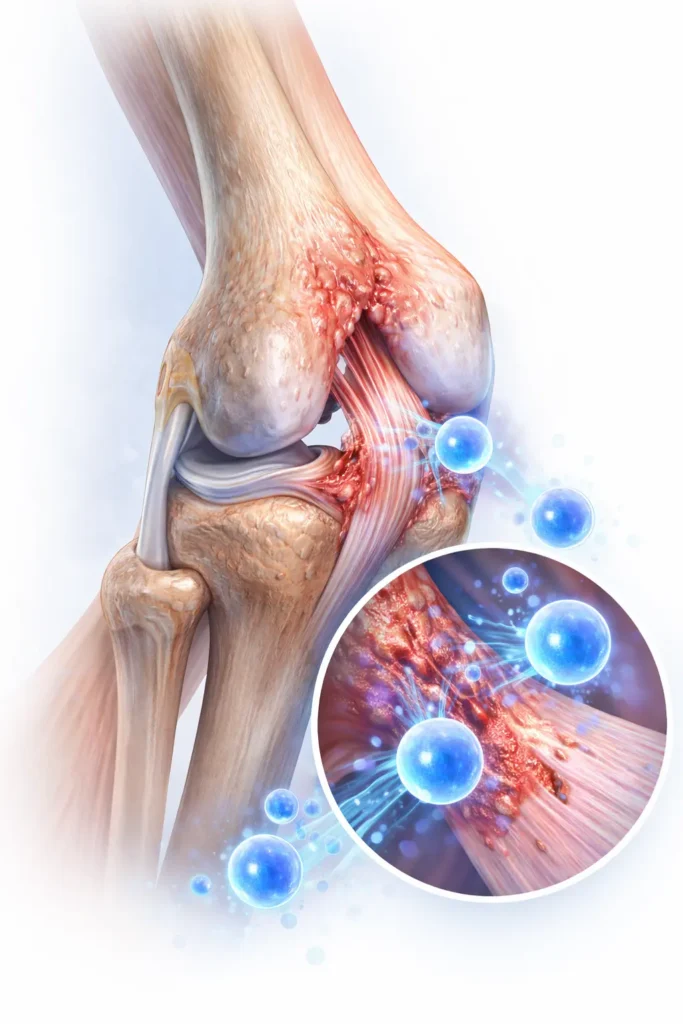
An ACL (anterior cruciate ligament) injury can cause knee instability, swelling, and loss of confidence during movement, especially in athletes and active individuals. Researchers are studying ACL stem cell therapy as an investigational, minimally invasive option that supports research into ligament tissue healing in cases of partial tears or degeneration.
What Is Stem Cell Therapy for ACL Injuries?
Researchers study stem cell therapy for ACL injuries as part of regenerative medicine research focused on supporting the body’s natural repair processes. For this reason, some patients with ACL injuries explore ACL stem cell therapy as an investigational, non-surgical option when conservative treatments—such as rest, bracing, or physical therapy—have not provided adequate recovery.
Additionally, providers discuss stem cell–based procedures in cases involving partial ACL tears or early ligament changes that contribute to knee instability. In these situations, some patients also explore stem cell therapy for knee pain as part of a broader evaluation.
How Stem Cell Therapy Works for ACL Injuries
Current research examines how stem cell–based approaches support ligament tissue affected by ACL injuries. At the same time, researchers study how biological signaling may influence inflammation, tissue remodeling, and joint stability following partial ligament damage.
What the Procedure Involves:
General Steps in Stem Cell Therapy for ACL Injuries
- Initial Evaluation & Imaging
A licensed provider reviews medical history, performs a focused knee examination, and may order imaging such as MRI or diagnostic ultrasound to assess ACL integrity, surrounding ligament structures, and joint stability. - Stem Cell Harvesting
Medical providers collect stem cells from ethically sourced tissue, such as bone marrow or adipose tissue, in a controlled clinical environment following established medical protocols. - Processing & Preparation
Laboratory specialists process the harvested tissue in a regulated setting to concentrate stem cells and prepare them for targeted administration. - Image-Guided Injection into the Tendon
Using ultrasound or fluoroscopic guidance, providers inject the prepared stem cells into or near the ACL and surrounding knee structures to support accurate placement and procedural safety. - Post-Procedure Monitoring & Follow-Up
After the procedure, medical staff monitor patients briefly, provide after-care instructions, and may schedule follow-up visits to assess symptom progression, knee stability, and functional recovery.
In general, stem cell–based procedures for ACL injuries involve harvesting stem cells from ethically sourced tissue, processing them in a controlled laboratory setting, and administering them to targeted knee structures.
In some cases, ACL injuries coexist with cartilage wear or early joint degeneration. Because of this, some patients also explore stem cell therapy for knee arthritis as part of a broader knee health evaluation.
At the same time, it is important to consider the following information.
Important Information
Actually, research is ongoing into how stem cells may:
- Support cellular signaling
- Contribute to tendon repair environments
- Interact with inflammatory pathways involved in ACL injuries.
ACL Conditions Studied in Stem Cell Research
In many cases, patients who inquire about stem cell therapy for ACL injuries often have knee instability, pain, or functional limitation related to ligament damage, degeneration, or prior injury. The following ACL-related conditions are commonly discussed in regenerative medicine research. Each condition is different, and eligibility depends on individual medical factors.
Partial ACL Tears
Partial tears of the anterior cruciate ligament may cause knee instability, swelling, and difficulty with pivoting or sudden directional changes. In these cases, researchers continue to study regenerative approaches as potential non-surgical options alongside structured rehabilitation.
Chronic ACL Laxity or Instability
Some patients experience ongoing knee instability following an ACL injury, even after initial healing or conservative care. Chronic ligament laxity may contribute to reduced confidence during movement and increased risk of secondary knee injury.
Post-Injury ACL-Related Knee Pain
Persistent knee pain may remain after an ACL injury due to altered biomechanics, compensatory movement patterns, or associated soft tissue involvement. Regenerative approaches are sometimes explored as part of a broader knee evaluation.
Post-Surgical ACL Symptoms
Some individuals experience lingering knee discomfort, stiffness, or functional limitation following ACL reconstruction surgery. In these cases, supportive regenerative strategies may be discussed during recovery and long-term joint management.
Who May Be a Candidate for Stem Cell Therapy?
Stem cell therapy for ACL injuries is not appropriate for everyone. A medical evaluation is required to determine whether this investigational approach may be suitable based on ligament condition, injury severity, treatment history, and overall knee health.
A patient may be considered for evaluation if they:
- Have a partial ACL tear or ligament-related knee instability
- Experience ongoing symptoms despite conservative treatment
- Are seeking non-surgical options
- Wish to delay or avoid ACL reconstruction surgery
- Understand the investigational nature of stem cell therapy
Risks and Limitations to Consider
While researchers continue to study stem cell–based therapies for ACL injuries, it is important to understand their current limitations and potential risks. Because individual responses vary, timelines remain uncertain and outcomes cannot be guaranteed.
-
Lack of standardized protocols:
Treatment approaches may vary between providers, as standardized clinical protocols for stem cell–based ACL procedures are still being developed. -
Variation based on injury severity:
Response may differ depending on factors such as the extent of tendon degeneration, tissue quality, injury chronicity, and overall musculoskeletal health. -
Uncertain and variable timelines:
Some patients may not experience noticeable symptom changes, and response timelines—if any—can vary from weeks to months. -
Possible risks and side effects:
As with any medical procedure, potential risks may include infection, inflammatory response, discomfort at the injection site, or lack of symptom improvement.
Why Patients Consider Stem Cell Therapy in Mexico
Some U.S. patients explore stem cell therapy options outside the United States due to differences in regulatory frameworks, access to investigational regenerative therapies, and cost considerations. Additionally, the availability of specialized regenerative medicine clinics influences this decision for some individuals.
When seeking care abroad, patients should prioritize education, medical screening, and provider experience as part of an informed decision-making process.
Rejuvacell Medical Group treats international patients while emphasizing:
- Patient education
- Medical screening
- Safety protocols
Medical Oversight & Experience
Licensed medical professionals evaluate stem cell–based procedures for ACL injuries within a structured clinical framework to support patient safety and appropriate medical decision-making.
All procedures are:
- Reviewed by licensed medical professionals
- Conducted under clinical protocols
- Evaluated on a case-by-case basis
Frequently Asked Questions
Is ACL stem cell therapy FDA approved?
ACL stem cell therapy is not FDA approved as a standard treatment. It is considered an investigational approach that researchers continue to study in regenerative medicine. Regulatory status may vary depending on how cells are processed and used, and patients should review these considerations with a qualified medical provider.
How long does the procedure take?
Stem cell–based procedures for ACL injuries are typically performed on an outpatient basis and generally take about 60 to 90 minutes, including preparation, image-guided injection, and brief post-procedure observation.
Can ACL stem cell therapy help avoid surgery?
Some patients with partial ACL tears or chronic ligament-related symptoms explore ACL stem cell therapy as a non-surgical option. While certain individuals may delay or avoid surgery, results vary, and this approach cannot guarantee that ACL reconstruction will be avoided. Complete ruptures may still require surgical repair.
How long does it take to notice changes after treatment?
Response timelines vary between patients. Some individuals report changes within several weeks, while others may take several months to notice differences, if any. Because ACL stem cell therapy is investigational, outcomes and timelines cannot be predicted or guaranteed.
Is imaging used during the evaluation and procedure?
Yes. MRI or diagnostic ultrasound is commonly used during the evaluation process to assess ACL integrity and surrounding knee structures. Ultrasound or fluoroscopic guidance is also frequently used during the injection to support accurate placement.
What the Patient Journey Typically Looks Like
Typically, patients begin with an initial consultation and medical screening to review symptoms, medical history, and imaging when appropriate. During this process, a medical provider evaluates ACL condition, injury history, prior treatments, and overall knee health.
If eligibility is determined, a personalized treatment approach may be discussed based on individual needs, clinical findings, and investigational protocols.
Request an ACL Consultation
If you are experiencing knee instability or an ACL injury and want to learn more about stem cell therapy, you may request a confidential consultation with a medical coordinator.
- No obligation
- Patient-focused discussion
- Medical review required